The long version of our mask study has been republished
A workshop report and some thoughts on it
Our mask study measured carbon dioxide levels in the inhaled air of 45 children wearing face masks. It found that the inhaled air under children’s face masks contained unacceptably high levels of carbon dioxide, about 1.3% to 1.4% by volume, or 13,000 to 14,000 parts per million. Normal outdoor carbon dioxide levels are 400 ppm or 0.04% by volume. The Federal Environment Agency and various protective regulations have determined that 2,000 ppm or 0.2 vol.-% is the upper limit above which damage to health cannot be ruled out. For children, such high values, as we measured after only 3 minutes, are absolutely unacceptable. Especially against the background that children are neither at high risk of corona infections and Sars-CoV2 nor are they important spreaders of infections.
The story
The study was published last year as a research letter in JAMA Pediatrics [1] and viewed nearly a million times. It sparked protest and was retracted by the journal under very questionable conditions; more on this below. Much of the negative feedback probably derived from the fact that the publication was an abridged version (with a 600-word limit) that contained important information only in small print – in the appendix and in the data sheets of the linked instrument descriptions – information that apparently not all critics had taken note of. We therefore endeavoured to publish the long version. Another journal was willing to initiate a new review process. After two long review processes with 3 reviewers each, where two gave positive votes and a third reviewer simply copy-pasted her negative comment on JAMA Pediatrics as a review and presumably gave a negative vote, the editors decided to reject it. We then went to a third journal, Environmental Research, a very good peer-reviewed journal outside the medical community. There, a new review process was initiated with 3 reviewers. One provided a factually useless review and voted for a revision. One apparently voted positively without any major requests for changes. One voted for a revision, which we then carried out, and was apparently also consulted again in a second round of review. After this second round, a few small things were criticized, which we incorporated, and now the article is published again [2].
Changes and more prominently presented information
Compared to the archived publication on the preprint server [3], there are some new features not included in the preprint version, which are essentially responses to criticisms made at some point by reviewers or critics. Of course, nothing has changed in the data and measurements themselves (except that we have rounded the measurement figures by the last two decimal places due to a reviewer’s request).
Technical details of the units
We have responded in the new publication to the fact that many of our critics have confused the data sheets of the two instruments we used, or have not even read them. In fact, two different measuring instruments were used, both from the same company. One was designed to measure indoor air and had a measuring range between 400 ppm and 5,000 ppm and was thus well suited to monitor the background carbon dioxide level, which we kept below 1,000 ppm by ventilating a lot. For comparison: The carbon dioxide level of the air outside is 400 ppm.
The actual meter used to measure the carbon dioxide content of the inhaled air had a sensitivity of 0 to 200,000 ppm or 0 – 20% by volume, making it ideally suited to map the values expected and found. It is designed to measure in medical contexts, such as in an incubator for babies. The accuracy of the measurement is 1% plus/minus after calibration. The latter is important because many critics have not understood what this means or have not bothered to understand it. If you calibrate the instrument to 5 vol.-% (because that’s all you can expect), then the measurement accuracy is 1% of that 5 vol.-%. (And how much is 1% of 5%, or one hundredth of 5%, dear Mr Fact Checker? Yes, that’s right, 0.05 %.) According to the manufacturer’s calibration certificate, it is 0.064 % by volume of the gas used for calibration (which is why the assessor obliged us to round the last two digits). This means: Values like the 1.3 to 1.4 vol.-% we measured are definitely within the sensitivity range of this instrument.
The device has a latency of 1 to 2 seconds. If, like us, you put a tube on it to deliver the carbon dioxide from the upper lip to the pump, the latency is 20 seconds. Many critics took this as an opportunity to say that it would not have been possible to measure the difference between inhaled and exhaled air because the latency time was too long. Such an argument is factually correct, but it implies a high degree of stupidity on our part and on the part of the experts. Dr Traindl, the measuring engineer who carried out the measurements, is a court-sworn expert for gas measurements and knows his business. Therefore, of course, we did not measure everything continuously, but we measured the different breathing phases separately. This was also described in the methodological supplement of our original publication, but perhaps not clear enough or too hidden.
Now it is clear, and I say it again here:
We only ever collected the air we were interested in in the meter and accumulated and averaged the collected measurements. Since we attached the measuring tube between the upper lip and the nose perpendicular to the flow of breath, the inhaled and exhaled air flowed past the measuring tube under the mask. There is a pump in the device that sucks in the air when pressed. A doctor continuously observed the child and actuated the measuring pump whenever a breathing cycle of interest, e.g. inhalation, began. This sucked inhaled air into the measuring device. When the inhalation phase was finished, he switched the pump off again; the remaining breathing phase was ignored. We collected the air from inhalation phases for three minutes, measured it every 15 seconds during each measurement and averaged the total of 32 values per measurement phase. After the inhaled air was measured, we measured the exhaled air. And before that, we measured continuously, inhaled and exhaled air together, for 3 minutes. We report all the data, but we were particularly interested in the carbon dioxide content of the inhaled air. And by separating the measurement into breathing phases, we can also say quite confidently that what we measured is really the carbon dioxide content of the air during inhalation under the mask. Anyone who doesn’t believe this should simply do a better study themselves. Besides, new data from other researchers have almost perfectly confirmed our data for FFP2 masks [4], I’ll get to that in a minute.
We have also discussed a possible objection in our new publication: One might say that there was still air of the previous phase in the measuring device when we measured the inhaled air. This is also an argument of critics. True, but these critics have also overlooked what was already stated in the earlier publication: We always made a pause of 30 seconds between the different phases. We discarded the data in this pause for precisely this reason. One could also argue that there is always a small difference between observing the start of a breathing phase, the triggering of the pump, and the real start of inhalation. This is also true, but at best this leads to a systematic error of displacement, which is made up for in the end and thus corrects itself.
The results: children breathe in an average of 14,000 ppm carbon dioxide under a FFP2 mask and 13,000 ppm under a surgical mask, in individual cases considerably more or less, but always more than the recommended limits. The newly published long version also contains a table in the appendix showing which masks we used. Namely, masks from different manufacturers, randomly mixed to compensate for a systematic bias effect of the masks.
We also note: The Federal Environment Agency sifted through all the data on carbon dioxide and health damage ages ago and came up with a standard [5]. 2,000 ppm or 0.2% by volume is the upper limit of what is acceptable for indoor carbon dioxide levels. At levels above this, adverse effects and even damage to health cannot be ruled out. Adverse effects are fatigue, concentration problems, headaches, etc. These and other problems have been documented in a survey of more than 20,000 children and their parents by our colleagues from the University of Witten: more than two thirds of the children suffer from such complaints after wearing masks [6]. Our values show: the safety margins of various standards, incidentally also the occupational health and safety standard [7], are violated by a factor of 6 to 7.
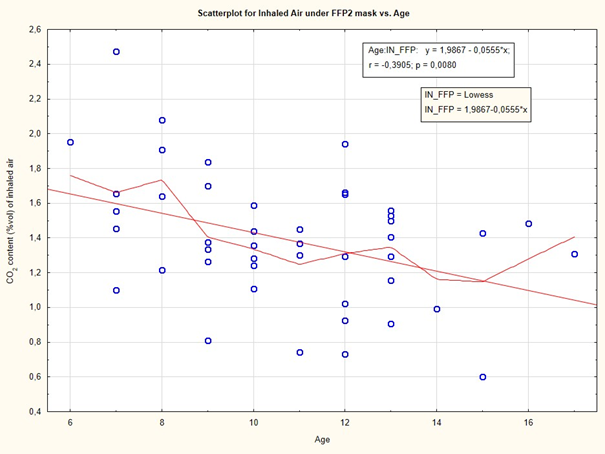
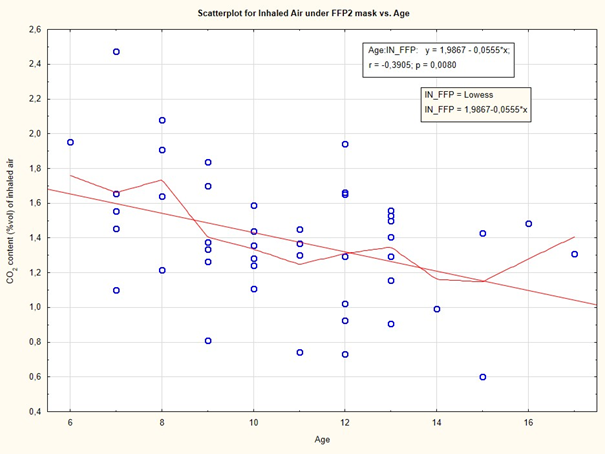
We were surprised ourselves that the differences between surgical and FFP2 masks are not as great as one would expect. We suspect that this is because children have small heads compared to the volume of the masks, and therefore surgical masks also retain a relatively large amount of carbon dioxide. As a result, the dead space volume, i.e. the space between the face and the mask, is larger for children compared to adults. The air breathed back therefore contains more carbon dioxide in children because their breathing volume is smaller relative to the amount of dead space in the mask. Therefore, until fresh air flows in, the carbon dioxide-rich air in the mask is inhaled first. This leads to the overall high carbon dioxide content.That this consideration makes sense is shown by our correlation calculation, depicted graphically in Fig. 1. Here we see that the carbon dioxide content in the inhaled air under the mask decreases in direct proportion to the age of the child: the older the children, the lower the carbon dioxide content. This is due to the overall larger breathing volume of older children and the fact that their dead space in the mask is smaller compared to their face size. However, it must also be said here: even the child with the lowest CO2 value, a 15-year-old boy, still had a value of inhaled carbon dioxide of 6,000 ppm, which was a factor of 3 above the limit value of 2,000 ppm.
Validation of measured values by calculation
In the new publication, we have added another calculation in the appendix. There is in fact an indirect method to verify the measurements, a so-called “back-to-the-envelope” calculation: back into the bag into which one blows, so to say. To do this, one uses the theoretical volume of the mask, the measured carbon dioxide content under the mask after exhalation, knowledge of the child’s age with a theoretical breathing volume and can then calculate how much carbon dioxide content the inhaled air contains. A previous assessor wanted these calculations. Dr Traindl did this for a total of 10 children. You can see that the theoretically calculated values and the measured values agree relatively well. The data are included in Supplementary Table 3 of the publication. Here is an excerpt:
| Child No | Age | Vol.% Measured | Vol.- % Calculated |
| 1 | 13 | 1.53 | 1.18 |
| 4 | 10 | 1.59 | 1.51 |
| 8 | 11 | 0.74 | 0, 77 |
A new study confirms our measurements
So these calculations indirectly validate our measurements. Perhaps a new, direct confirmation is even more impressive. One criticism of our study was that we had not used the right measurement method. We should have measured with capnography. Capnography measures the carbon dioxide content at the end of the exhalation phase. From this, the inhaled carbon dioxide content can be calculated. Capnography is used in emergency medicine and anaesthesia to monitor a patient’s vital state and is of course very well established there.
But it is hard to see why one has to use a method just because it is well established and better known. It has always been my methodological principle to do what is appropriate to a question, not what is commonly known. The latter is like the story of Nasreddin Hodja, who was observed by a neighbour searching around in the dark under a lamp. Asked what he was doing, he said he was looking for his key. Had he lost it there? No, but it is where the light is, Nasreddin said.
Kapnography is well known. That is an advantage. A disadvantage is the fact that it does not measure carbon dioxide levels when you inhale, but when you exhale, and you have to calculate the amount of carbon dioxide inhaled first. This has now been done by a new study recently made available on the preprint server MedRxiv.org [4]. Martellucci and colleagues measured carbon dioxide under face masks in 102 participants who were between 10 and 90 years old. Ten of them were children, 20 were elders and 72 were adults. Inhaled carbon dioxide levels were calculated and reported for children, adults and elders as follows.
| Children | Adults | Elders | |
| Without | 457 | 461 | 450 |
| OP mask | 6,439 | 4,852 | 4. 638 |
| FFP2 mask | 12,847 | 9,056 | 8,894 |
We see: Under FFP2 masks, the values agree relatively well with what we measured. We measured 14,000 ppm, Martellucci and colleagues back-calculated just under 13,000. Under surgical masks, the difference is greater: we measured 13,000 ppm, Martellucci and colleagues calculated just under 6,500. There could be several reasons for this. When exhaling, the resistance is perhaps lower with surgical masks. Perhaps there are other reasons. The Italian group measured at the lower lip, while we measured between the upper lip and the nose. We think our measurement point is more favourable.
The whole set-up was similar to ours, with a few differences: The measurements lasted 10 minutes, whether in total or for all conditions is not quite clear from the diagram. Measurements were taken three times, after three, four and five minutes, so with much lower data density than we had. The so-called “end-tidal volume”, i.e. the CO2 content at the end of an exhalation phase was measured and from this, similar to our “back-to-the-envelope” calculation, the inhaled CO2 level was calculated.
Overall, it seems to me that our measurement method is more sensitive to what we want to know. Most importantly, our data is based on measurements rather than calculations. But even this study shows that mask use in children and adults leads to high levels of carbon dioxide in the air we breathe.
Further considerations and data
Dr Kampf, a hygienist from Hamburg, has written a highly recommended book titled “Wissenschaft ist frei. Auch in der Pandemie?” (“Science is Free. Even in the Pandemic?”) [8]. Hygienists are actually the ones who understand the most about hygiene and measures to fight and contain infections. I worked for a few years at the Chair of Hospital Hygiene with Prof. Daschner in Freiburg and learned a lot about the subject there. Unfortunately, hygienists hardly ever had their say in this corona crisis and when critical statements were made, they were ignored or trivialized by “fact checks”. Dr Kampf points this out. This book contains a very readable chapter on masks. The overall verdict is sceptical. At best, masks have a place in very circumscribed contexts, but not at all in everyday life, and certainly not for very unspecific prevention. This is because the health-endangering effects must be weighed very carefully against the protective ones. The health hazards include not only the increased carbon dioxide content of the inhaled air but also hygienic problems: All kinds of pathogens collect in the masks, even after a short time, which are breathed back and can lead to other infections. The fabric often contains questionable additives that do not belong in the air we breathe. These harmful effects are permanent and cumulative. Some of them may even be very alarming. For example, children, whose brains and organisms are still growing and thus have higher oxygen requirements, especially when they are supposed to be learning, get too little of it.
A just-published study comparing districts in Kansas with mandatory masks against those without found that 50% more people died of SARS-CoV2 in the districts with mandatory masks, because infectious particles collect through the masks and only then grow to a problematic amount [9]. Whether this result is reliable is difficult to judge. In any case, the apparently unquestionable usefulness of face masks should be subjected to careful scrutiny.
While the problems of masks have been widely documented and are now also known through MIES – Masked Induced Exhaustion Syndrome – in a systematic review [10], their benefits have only been marginally proven. The studies that are often cited suffer from the fact that the methodological quality of the summarized studies is poor [11, 12]. Newer, better reviews [13, 14] are often simply ignored. And individual studies based solely on model calculations [15, 16] are overrated. Their results only have relevance if the input parameters are reasonable and thus model a situation that is realistic. The study from the working group of Dr Bodenschatz at the MPI in Göttingen, for example [16], even though it was published in PNAS and thus in an excellent journal, is irrelevant and useless for decisions in the context of general prevention. It assumes a viral load in the exhaled air of a potential source of infection from a Chinese study and from a French study from the early days of the pandemic. In order to get to the original source, one first has to dig through two self-citations of other own studies in the publication, because this information is not included in the publication at all. This “viral load” is one of the highest ever measured and comes from terminally ill patients. At the University of Witten-Herdecke, this study was used as an argument for using FFP2 masks in lectures. How realistic is it, I ask, to have a terminally ill Covid-19 patient sitting in a lecture hall spewing a uniquely high viral load (because he is not using a mask)?
A Japanese simulation study is also often cited [15]. At first glance, it provides clear evidence for the effectiveness of face masks. The simulation is also based on extremely high viral loads as measured in terminally ill patients. Now, in this simulation, these terminally ill patients are placed as plastic heads in a box with a volume of 50 cm (distance) by 20 cm by 30 cm, i.e. with a cubature that is completely insane because it never occurs in reality. And so that the artificial measuring heads also come into contact with viruses, they are artificially snorted for another 20 minutes and then measured, i.e. a long interaction time is simulated under completely crazy conditions. To find the information on these conditions, however, you first have to eat your way through a supplement. Because the publication does not contain these specifications.
Such simulations, which at first glance look very convincing because they contain complex calculations and nice bar graphs, have largely dominated the debate, while properly done realistic measurements or more complex realistic studies such as the Danish mask study, which showed no effects at all [17], have been ignored and discredited by self-appointed fact-checkers. As is well known, our mask study was fact-checked for German Television (ARD) by Mr Rohwedder, who is an equestrian sports reporter and thus certainly a proven expert on experimental carbon dioxide measurements. He ruled the study to be bad. And because this fact check was so viable, the German Medical Journal immediately picked it up, since the editors there apparently found the competence of an ARD fact-checker with “equestrian sports” as a certificate of competence sufficient to form a professional opinion.
I say this mainly to make it understandable how such crazy and actually harmful measures as widespread mask-wearing in low-prevalence situations could become a supposed cultural achievement, so that you can no longer ride a train or go to the bathroom in restaurants without a mask. It’s because useless but prominently published (and also much easier to get to) papers in high-profile journals dominate the discourse. This is because those who shape it, science journalists and television journalists, understand little of the content and go mainly for formal criteria – who made the publication, which institution supports it and where did it appear. But that, as I have just shown, does not necessarily guarantee the truthfulness or relevance of a publication.
A large Finnish study has just shown, comparing two large Finnish cities, Turku and Helsinki – in Turku mandatory masks for children between 10 and 12, in Helsinki not – that, if anything, a greater incidence of infection was observed in Turku with mandatory masks for younger children, but no evidence whatsoever of any infection-related containment of incidence by mandatory masks [18].
So, gentlemen and ladies of the ARD editorial staff, of the fact-checkers’ guild and other friends of face masks: face masks increase the carbon dioxide content of the inhaled air in children (but also in adults). There is no getting away from that, even if it is politically incorrect. Dear high school boards, headmasters and teachers: In my opinion, given this outcome, whoever requires children to put on masks, commits bodily injury.
The argument that teachers must be protected is without reason. Because – data and references to this can be found in our study – children are no relevant spreaders of Sars-CoV2 infections. Even if it were so, one could better selectively close a class or exempt a teacher from normal duties for as long as necessary to protect their health. But the widespread general prescription of masks is not a proportionate preventive measure because the harm has been documented, and the benefit has never been proven. If someone disagrees, it is on them to prove the benefit and show that the harm argument is irrelevant.
Whoever then starts to argue with individual cases that are documented, please also accept the individual case argument on the effectiveness of homeopathy or on the proof of the existence of the Virgin Mary. The latter has been sighted in individual cases. Homeopathy knows of hundreds of thousands of individual cases that it has cured. Nevertheless, this is not accepted by science – and rightly so – as an argument that the effectiveness of homeopathy has been proven. In the same way, one cannot use individual cases to prove the danger that allegedly emanates from children and then enact a general mask requirement for children. Pardon, one can. But then one should say: Rationality and scientificity are not relevant for us.
I propose: We stop this nonsense extensively. To prevent infections, the usual measures are enough: Those who are ill stay at home. Those who are very afraid can continue to walk around with a mask. But everyone should know that they are not doing themselves any favours. In areas of high risk, it is acceptable. But in ordinary everyday situations, from supermarket to school, from train to open-air cinema? Nonsense squared.
Guilt by proximity and dubious financing?
Oh yes, in case someone now no longer knows how to criticize the study factually and therefore wants to switch to the popular sidetrack “guilt by proximity, dubious financing” in order to be able to criticize after all:
The study was cheap and cost about 5,000 euros all together. Most of it went to Dr Traindl, who was able to buy the measuring device from it, which was new, and was reimbursed his expenses for travelling from Vienna. We stated this in the Conflict of Interest statement of the publication. The expenses were funded by the MWGFD, which funds itself entirely from private donations, receives no industry money, no money from Russia or from outer space. No, not even from Soros and Gates. The MWGFD has also taken over the fees for online publications. And no, the MWGFD is not a lobby group of any political or economic group. It is not funded by the financially powerful anti-vaccine mafia, nor by the Nazis on the far side of the moon. Rather, it is what the name implies: an association of scientists and doctors committed to freedom, democracy and health in a holistic sense.
I myself generate my income exclusively on a freelance basis through consulting, and the homeopathic industry is not one of my clients and does not pay me any money for saying that homeopathy works but has no causal mechanism, but one that we have not understood, more on that in one of my next blogs. My endowed chair, funded by the Heel company, expired in 2016 after the faculty closed our course [19]. The blog I wrote for homeopaths until 2020, which was funded by an endowment, was – see above – no longer funded due to my involvement with Corona.
I have invested an estimated 14 days of time in this study, close calculations (preparation, organization, protocol development, evaluation, writing, revising, submitting, replying to critiques, resubmitting and rewriting, etc.). At my usual daily rates, that would be about 14,000 euros that I didn’t get paid for, but donated to the public.
Sources and literature
- Walach H, Weikl R, Prentice J, Diemer A, Traindl H, Kappes A, et al. Retracted: Experimental assessment of carbon dioxide content in inhaled air with or without face masks in healthy children: A randomized clinical trial. JAMA Pediatrics. 2021.
- Walach H, Traindl H, Prentice J, Weikl R, Diemer A, Kappes A, et al. Carbon Dioxide Rises Beyond Acceptable Safety Levels in Children Under Nose and Mouth Covering: Results of an Experimental Measurement Study in Healthy Children. Environmental Research. 2022;in print.
- Walach H, Weikl R, Prentice J, Diemer A, Traindl H, Kappes A, et al. Carbon Dioxide Rises Beyond Acceptable Safety Levels in Children Under Nose and Mouth Covering: Results of an Experimental Measurement Study in Healthy Children. Archiveorg. 2021; https://archive.org/details/Carbon-Dioxide-Face-Masks.
- Martellucci CA, Flacco ME, Martellucci M, Violante FS, Manzoli L. Inhaled CO2 concentration while wearing face masks: a pilot study using capnography. medRxiv. 2022:2022.05.10.22274813.
- Umweltbundesamt. Gesundheitliche Bewertung von Kohlendioxid in der Innenraumluft [Health assessment of carbon dioxide in air within closed rooms]. Bundesgesundheitsblatt – Gesundheitsforschung – Gesundheitsschutz. 2008 2008/11/01;51(11):1358-69.
- Schwarz S, Jenetzky E, Krafft H, Maurer T, Martin D. Coronakinderstudien “Co-Ki”: erste Ergebnisse eines deutschlandweiten Registers zur Mund-Nasen-Bedeckung (Maske) bei Kindern [Corona children studies “Co-Ki”: First results of a Germany-wide registry on mouth and nose covering (mask) in children]. Monatsschrift Kinderheilkunde. 2021;169:353-65.
- Institut für Arbeitsschutz der Deutschen Gesetzlichen Unfallversicherung. Datenblatt Kohlendioxid [Datasheet Carbon Dioxide]. IFA Gestis Stoffdatenbank. Berlin: DGUV – Geutsche Gesetziche Unfallversicherung; 2021.
- Kampf G. Wissenschaft ist frei. Auch in der Pandemie? Hamburg: tredition; 2021.
- Fögen Z. The Foegen effect: A mechanism by which facemasks contribute to the COVID-19 case fatality rate. Medicine. 2022;101(7):e28924.
- Kisielinski K, Giboni P, Prescher A, Klosterhalfen B, Graessel D, Funken S, et al. Is a Mask That Covers the Mouth and Nose Free from Undesirable Side Effects in Everyday Use and Free of Potential Hazards? International Journal of Environmental Research and Public Health. 2021;18(8):4344.
- Chu DK, Akl EA, Duda S, Solo K, Yaacoub S, Schünemann HJ, et al. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis. The Lancet. 2020;395(10242):1973-87.
- Liu IT, Prasad V, Darrow JJ. Evidence for community cloth face masking to limit the spread of SARS-CoV-2: A critical review. Cato Institute Working Paper. Washington DC: Cato Institute; 2021.
- Jefferson T, Del Mar C, Dooley E, Ferroni E, Al-Ansari LA, Bawazeer G, et al. Physical interventions to interrupt or reduce the spread of respiratory viruses. Cochrane Database of Systematic Reviews. 2020;CD006207.pub5.
- Xiao J, Shiu EYC, Gao H, Wong JY, Fong MW, Ryu S, et al. Nonpharmaceutical measures for pandemic influenza in nonhealthcare settings – personal protective and environmental measures. Ermerging Infectious Diseases. 2020;26(5):967-75.
- Ueki H, Furusawa Y, Iwatsuki-Horimoto K, Imai M, Kabata H, Nishimura H, et al. Effectiveness of Face Masks in Preventing Airborne Transmission of SARS-CoV-2. mSphere. 2020;5(5):e00637-20.
- Bagheri G, Thiede B, Hejazi B, Schlenczek O, Bodenschatz E. An upper bound on one-to-one exposure to infectious human respiratory particles. Proceedings of the National Academy of Sciences. 2021;118(49):e2110117118.
- Bundgaard H, Bundgaard JS, Raaschou-Pedersen DET, von Buchwald C, Todsen T, Norsk JB, et al. Effectiveness of Adding a Mask Recommendation to Other Public Health Measures to Prevent SARS-CoV-2 Infection in Danish Mask Wearers. Annals of Internal Medicine. 2020;174(3):335-43.
- Juutinen A, Sarvikivi E, Laukkanen-Nevala P, Helve O. Use of face masks did not impact COVID-19 incidence among 10–12-year-olds in Finland. medRxiv. 2022:2022.04.04.22272833.
- Walach H. Sozialer Mord – “ein Mord, den jeder begeht”? Ein Schelmenstück in fünf Akten. In: Mäckler A, editor. Schwarzbuch Wikipedia Mobbing, Diffamierung und Falschinformation in der Online-Enzyklopädie und was jetzt dagegen getan werden muss. Höhr-Grenzhausen: zeitgeist; 2020. p. 77-107.